Hip disorders
Anatomy
The hip is largest joint in the body. The following pages set out the basic anatomy of the hip in order to help you understand what happens in disease processes and how surgery can be performed to alleviate symptoms.
The hip joint
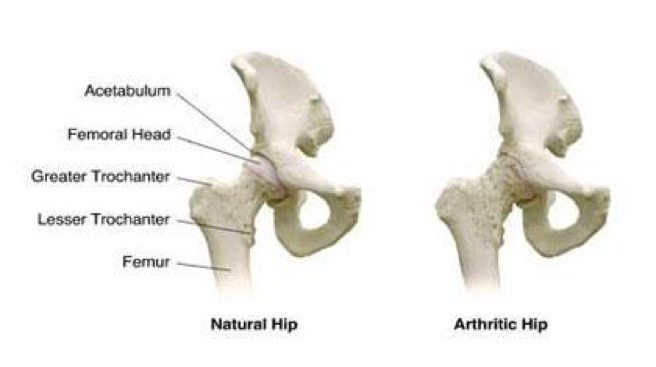
The hip joint is a ball and socket joint. The femoral head (ball) sits in the acetabulum (socket). Underneath the femoral head lies the femoral neck. Two prominences in the upper part of the femur, the greater trochanter and the lesser trochanter, allow the attachment of muscles onto the bone.
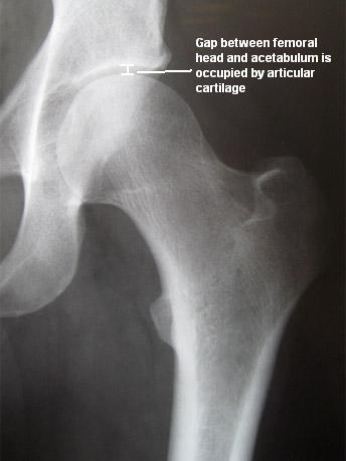
The joint surfaces are covered by several millimetres of articular cartilage, which can be seen as a gap between the bones on the following hip X-ray.
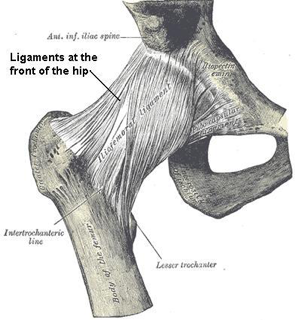
The Hip joint is enveloped by thick ligaments binding the femur and acetabulum together. At the front the ligaments extend down on the line between the greater and lesser trochanter (intertrochanteric line) and at the back of the hip the ligaments insert much higher up onto the femoral neck.
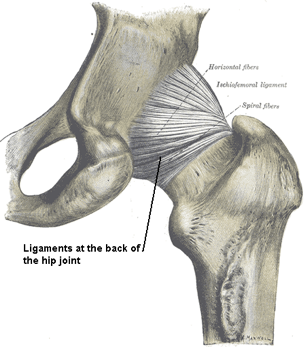
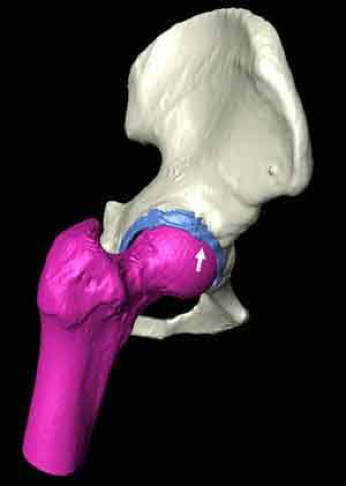
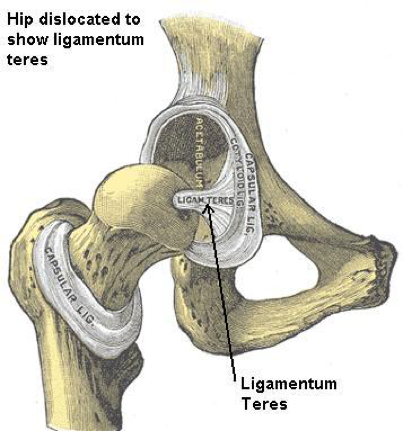
The head of the femur is connected to the acetabulum by an internal ligament (ligamentum teres) which is probably more important as a blood supply to the femoral head during growth.
Types of disorder
Many disease processes can affect the hip and knee. The following pages discuss some of the common conditions that cause symptoms and often require surgery.
Osteoarthritis
Osteoarthritis (OA) refers to degenerative (wear and tear) change that can occur in any joint in the body. When arthritis develops the articular cartilage (lining cartilage) is slowly rubbed away eventually leading to bone on bone contact.
So called secondary OA can occur due to a misshapen joint which may follow from fracture or trauma or due to abnormalities of growth (eg dysplasia and perthes). Femoro-acetabular impingement is another condition that is thought to lead to OA. The abnormal shape causes abnormally high stresses in the joint and over time leads to cartilage damage and degeneration. Primary OA occurs in the absence of any trauma or shape abnormality.
There may be hereditary (genetic) factors and/ or environmental factors that predispose to the development of primary OA. There is a great deal of research ongoing to try to understand the causes of primary OA.
Rheumatoid Arthritis
Rheumatoid arthritis (RA) is an inflammatory joint disease which usually affects many joints at the same time. It is characterised by inflammation and swelling. It tends to affect people at a younger age than osteoarthritis. Research suggests that it is mediated by an auto-immune process which means that the body’s own immune system attacks and destroys the joint surface.
There are many medical treatments for patients with RA and in recent times these have become so successful that we are seeing less patients progressing to the point of needing joint replacement.
Dysplastic hips & CDH
The word ‘congenital’ refers to abnormalities occurring during foetal growth and therefore imply failure of the body to develop properly. The most common example in relation to the hip is congenital dislocation of the hip (CDH), when a baby is born with a dislocated hip joint.
A less severe form of the same process is referred to as developmental dysplasia of the hip (DDH). The hip joint fails to develop fully so that the acetabulum is shallow and the femoral head is not fully contained in the hip. Often in patients with dysplasia the hip can be completely without any symptoms (asymptomatic) until the onset of symptoms in early adulthood (20s and 30s). The acetabular roof is more vertical and the femoral head lies in a more lateral position (reduced centre edge angle). High stresses on the lateral acetabular margin cause wear of the articular cartilage.
Patients with dysplasia who have not yet developed osteoarthritis but do have symptoms from their hip are sometimes offered surgery to correct the alignment of the acetabulum.
Trauma
Severe trauma or injury can result in fracture of the femoral head, neck or acetabulum. Intra-articular fractures can be serious as the joint surfaces are disrupted. If the fracture heals with some resulting displacement then this irregularity of the joint surface may result in fairly rapid degenerative changes.
Alternatively, the blood supply to the femoral head may be disrupted (Avascular Necrosis or AVN) in which case the femoral head may collapse causing pain and secondary arthritis.
Sometimes chronic or repetitive trauma, for example in a professional athlete or sportsman may result in articular cartilage damage and arthritis A chronic or repetitive injury could be caused by a professional athlete such as a footballer sustaining a lot of smaller injuries.
The net effect is to disturb or disrupt or damage the cartilage of the joint.
Infection
Infection involving the joint is quite rare. It was more common a hundred years ago when tuberculosis was widespread. Infection can occur in neonates (babies), children or sometimes after therapeutic injections. The net effect of infection is to cause damage to the cartilage and surrounding tissues and its damage results in arthritis.
Ligamentous laxity
There is considerable variation in how lax or mobile people’s joints are but there are some conditions where the joints are abnormally lax and this can be associated with a variety of rare disorders such as Ehlers-Danlos syndrome and Marfan’s Disease. When joints are exceptionally mobile the joint can be damaged as the joint partly moves out of position (subluxation).
Avascular necrosis
Avascular necrosis (or osteonecrosis) describes a condition whereby the blood supply to the femoral head is temporarily disrupted.
This temporary arrest of blood flow can occur as a result of serious trauma such as a hip fracture or dislocation but can also occur as a result of taking medication, particularly corticosteroids.
The blood supply of the femoral head is reduced which causes localised bone death (bone is a living structure). The process normally causes acute and severe pain and later on within a few weeks or months the bone is taken away or resorbed to be replaced by new bone. It is at this later stage where the process of removing the dead bone causes a weakness of bone just underneath the articular cartilage (subchondral bone).
This can result in collapse (subsidence) of the adjacent articular cartilage, joint surface incongruity and later secondary arthritis.
X-ray showing subchondral fracture of the left femoral head due to osteonecrosis or AVN

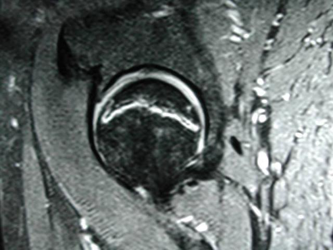
MRI scan showing high signal in the femoral head
Femoro-acetabular impingement
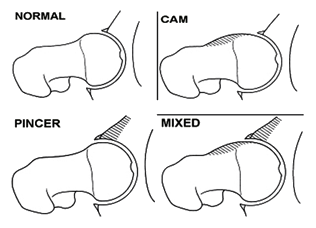
Research over the last 10 years has suggested that small abnormalities in the shape of both the femoral head and the acetabulum can result in damage to the articular cartilage to the hip and the labrum. This has been called hip impingement or femoro-acetabular impingement(FAI) and there are two main forms.
The first is CAM type impingement where there is an abnormality at the junction between the femoral head and neck such that this area is no longer concave (dished or sculpted). When the hip flexes the hip acts as a cam and tries to force the abnormal area into the socket damaging the cartilage and the labrum.
The second type of impingement is called PINCER impingement. In this type the abnormality is in the socket which may be too deep, or angled backwards (retroverted) rather than forwards (anteverted). Again, when the hip flexes damage to the labrum occurs as it hits against the femoral neck. Recent work has suggested that cam and pincer impingement often occur together.
Symptoms of impingement are groin or hip pain that occurs on flexion or flexion and rotation.
Tears in the labrum can result in clicking or catching type symptoms. Surgically treating these abnormalities alleviates the symptoms and may perhaps stave off the development of osteoarthritis.
Slipped Upper Femoral Epiphysis (SUFE)
Long bones have areas where rapid growth can occur. In the femur, there are two areas, the upper and lower femoral epiphysis. During the growth spurt (between the ages of 10 and 12) the upper femoral epiphysis is active and the cartilage in this area is thicker and mechanically weaker than the surrounding femoral bone.
Occasionally a fracture can occur through this weak area separating the growth zone. This requires surgery to fix the fracture with screws. Often a slight deformity at the region of the fracture can persist into adulthood and this may be one cause for femoro-acetabular impingement (FAI).
Symptoms
Nearly everybody will experience aches and pains in their joints at some time. This is not to be confused with more serious joint disorders.
Osteoarthritis is often a slow process and symptoms can vary quite significantly.
Quite often stiffness and slight lack of flexibility is the first noticeable problem. This can occur over many years and is not often perceived to be disabling by the patient.
Any pain that is experienced is often aching in nature and usually occurs towards the end of the day or after exercise. It is not uncommon for this early phase to last several years.
The stiffness may slightly increase and this stiffness starts to become noticeable and impact in terms of activities of daily living.
Common symptoms caused by stiffness of the hip include:
- Difficulty putting shoes and socks on
- Difficulty cutting toenails
- Difficulty getting in and out of the car
- Difficulty walking at a reasonable pace
- Difficulty coping with stairs
- Difficulty going up or down inclines
- Difficulty getting in and out of the bath
There are many more examples.
Often hip pain starts off as a dull ache and is intermittent or periodical. Gradually the pain can increase in terms of how long it lasts and its type and severity. Pain is particularly troublesome if it occurs at night.
This interferes with sleep and when patients cannot get a good night’s sleep their whole quality of life starts to become intolerable. The pain can become very severe, particularly pain experienced deep in the groin.
Pain is also often experienced in the buttock and is also quite commonly felt to spread down the thigh towards the knee.
Some patients can present to the doctor convinced the problem is in the knee but in fact the disease is in the hip.
This distribution of pain is known as referred pain in that the pain in the hip is referred to the knee.
There are some practical limitations that arthritis can impact on.
Here are some examples:
- Difficulty coping with housework
- Difficulty coping with shopping
- Difficulty working
- Difficulty coping with personal hygiene
- Difficulty with physical relations
- Difficulty driving for any length of time
Psychological effects
The combination of pain, stiffness and limitation of activities quite understandably can cause unhappiness and distress, not just to the patient but to carers and relatives as well.
Certain psychological disorders such as anxiety or depression can be a bi-product of joint disorder. If you feel affected in this way please consult your GP.
Combatting joint disorder
The following suggests particular common methods of dealing with joint disorders, from joint pain to stiffness and the inability to conduct certain activities:
Tablets
Many patients are reluctant to take tablets. Why? Here are some common reasons:
“I don’t like taking tablets”
“I don’t want to become addicted to tablets”
“Tablets don’t agree with me”
“Tablets upset my stomach”
“These tablets give me constipation”
“I am frightened by the long term effect of taking tablets”
Common medications
Paracetamol - usually the best tablets to start with. (Please be aware of not exceeding recommended doses). It is best to start with intermittent or as and when needed. This can lead to more regularly sustained medication.
Your doctor can advise you on stronger tablets than Paracetamol with combined other agents such as Codeine.
Non-steroidal anti-inflammatories(NSAIDs) - these are quite similar to Aspirin. Common tablets include Ibuprofen, voltarol (diclofenac) and naproxen. These tablets act differently to Paracetamol by reducing the effects of inflammation. They can often cause stomach upset or more serious complications, particularly in susceptible or elderly patients.
Other medications
Glucosamine & Chondroitin sulphate.
Some patients find that they gain benefit from taking glucosamine or chondroitin although there is little strong scientific evidence that they are effective, particularly in more serious joint conditions.
They are unlikely, however, to do any harm and may provide symptomatic relief in mild to moderate Osteoarthritis.
Exercise & weight
It is safe and in fact it is recommended to carry out light exercise as this improves the quality of the muscles and bone.
It is best to avoid exercises which involve potential injury to the joint - such as impact exercises or exercises including running particularly on hard ground. Safer exercises include swimming and cycling.
Arthritis will be made worse by excess weight as it will put higher stresses on the joints. However, many patients find they cannot exercise due to their arthritis and consequently tend to put on weight.
Weight reduction can reduce pain significantly and this can be achieved if not by exercise than with dietary methods.