Heading for surgery
Surgery is not the first option in dealing with arthritis.
Any operation is invasive and can carry risks as well as benefits. In the early stages, arthritis is more of a nuisance than a disability and therefore sensible measures such as a well balanced diet, low impact exercise and if necessary modification of lifestyle is important. If the pain becomes more severe it is often necessary to take some painkillers.
When the symptoms, i.e., pain and/or stiffness and/or disability become more troublesome, then surgical solutions can be discussed with your surgeon.
In our view, this is probably the most important and educational part of the process. It is a time when expectations are set and agreement is made between the patient, General Practitioner and specialist.
It is also a very important part of the process of consent and it is a time when most patients are eager to know the options, benefits and risks of surgery. (See the consent section).
Potential benefits
Pain relief
The operation may relieve all the associated pain and it is certainly quite possible and not uncommon for patients to resume almost completely normal function following hip replacement surgery.
However, it is not uncommon to have some residual tenderness around the wound for some months and even thereafter some minor discomfort may persist.
Mobility
Range of movement should improve following surgery but full movement may not be restored. Regarding the hip, restrictions may be placed on you for several weeks to reduce the risk of dislocation.
Function is usually improved following surgery in terms of walking ability, speed of walking and light exercise. You may wish to discuss with your surgeon what sort of exercises and activity and sports may be possible after your operation.
This to some extent depends not just upon the operation but also in terms of general fitness and pre-operative activity levels.
Quality of life
Hip replacement is well recognised as being one of the most successful operations at improving quality of life.
This is because the pain and impairment of function from hip arthritis affects almost all aspects of the patient’s life including basic activities of daily living (washing, dressing etc.), ability to work, leisure activities, sleeping and social relationships. Following surgery patients feel improvement in these areas with a consequent improvement in quality of life.
Things to consider
It is important to consider any negative impact of an operation in terms of potential complications of an operation.
Here are some considerations:
- What are the risks of the operation?
- Could the operation make me worse?
- What sort of limitations can I expect after the operation?
- How long will it take to recuperate?
- How long will the benefits of the operation last?
- If the operation went wrong and further surgery was necessary what would this involve and what risks would that secondary intervention impose?
- If I decide not to have the operation will I be making the eventual operation more difficult, i.e. will I damage the joint further?
You should feel free to ask questions to your surgeon, GP or therapist prior to considering an operation.
Not all patients and surgeons have exactly the same thresholds of advising patients as to when an operation is appropriate. In general terms an operation is considered when other conservative or non-operative measures are no longer effective, when pain starts to become very intrusive or when pain starts to affect sleep and when activity is such that the overall quality of life is compromised.
On the other hand, some patients value their activity very highly and may consider having an operation such as hip replacement at a slightly earlier stage to maintain their functional status, i.e. stay at work and to stay active prior to losing their activity (threshold for surgery).
Consent
Before going ahead with an operation, the surgeon must obtain consent from the patient, that is the consent to operate.
The process of obtaining consent is that the surgeon must explain and be satisfied that the patient understands the reasons for carrying out an operation, the potential advantages and the potential disadvantages or complications of the procedure. This involves a discussion about the whole process.
In this context, it is necessary to understand the natural history of the disease if an operation is not carried out, i.e. if continued conservative measures are taken and also what would happen if an operation is carried out in terms of the improvement in quality of life, pain reduction, mobility etc. and any downsides to the operation and the nature of these complications.
This whole process is quite complex, particularly when considering fairly major surgery and different patients have different rates and capability of processing this information and different surgeons have potentially different styles in conveying the information.
There are many different sources of information available to patients.
Clearly a face to face consultation with the surgeon is the mainstay but there are also patient information leaflets, websites and of course television and radio. It can sometimes be difficult for patients because there is too much information and they can feel overwhelmed. Sometimes it is necessary to discuss things with your surgeon on more than one occasion prior to making a definitive decision about surgery.
Complications
Very few people would like to think what could go wrong, either during or following a surgical procedure to replace the hip or knee joint. However, it is important that patients are made aware of potential risks so that they - the patient - can ultimately decide whether surgery if for them. The patient (with help from the surgeon) must weigh up the potential advantages against the potential disadvantages of any procedure before deciding to go ahead (and so consent). After all, this is what we do before we make any important decision whether it be in healthcare, business or domestic decisions.
Remember, don’t be afraid to ask questions, even more than once. There are potentially many questions but in the main then include:
- What (in lay terms) is the nature of any potential complication?
- What are the chances of developing a complication?
- If the complication occurs what could be done to remedy it?
- What are the chances of fixing it, either completely or partially?
In relation to joint replacement surgery complications are sometimes considered general complications and then specific to the joint. Complications can also be considered relatively early, within a matter of six weeks to 12 weeks and those occurring at a later time, perhaps years after the original surgery.
In relation to general complications there is a risk of death (in the region of 2 in 1,000 to 6 in 1,000 depending on age at the time of surgery), medical complications, for example myocardial infarction (heart attack), cerebrovascular accident (stroke), chest infection, urinary tract infection and complications related to immobility such as a pressure sore, deep venous thrombosis (blood clot in leg), pulmonary embolism (blood clot in the lung).
Complications specific to joint replacement would include a wound infection, either superficial just involving the skin or a deep infection involving the implant, (in deep infection there may not always be a superficial infection component), dislocation, post-operative leg that is either longer than normal or shorter, nerve injury of the sciatic nerve, femoral nerve, very rarely vascular injury, heterotopic ossification or bone formation around the hip.
Later complications include loosening of the fixation, wear of the joint and bone loss around the femur and acetabulum, mainly as a consequence of loosening and wear and the necessity of the revision surgery.
Before surgery
The operation may be within a couple of weeks, alternatively it may be three or four months off depending on the precise circumstances. Patients often ask what they should do at this stage. The broad advice is to stay as healthy as you can.
If you are a smoker you should avoid smoking as smoking significantly interferes with respiratory function following surgery.
Avoid excessive alcohol intake. Eat sensibly. It is probably not wise to go on a crash diet as this has a potentially adverse metabolic effect but equally avoid overeating.
Sensible exercise, obviously, pain may prevent you from exercising in some circumstances, but continue muscle action such as walking. Don’t become a couch potato!
Try and ensure you have not got any areas of active infection. It may be worth visiting a dentist to have your teeth checked out to make sure there are no areas of dental sepsis. Keep an eye on your skin for any infections and any urinary tract infections, if you are prone to urinary tract infections.
Time off work
There will be several arrangements to make either with your partner, family and work.
Quite commonly, patients are off work for up to three months following a hip replacement but with less active forms of work patients may get back to work within six weeks, possibly less. It does vary and you need to consider your own exact circumstance.
You should already be considering what happens after the operation to make any other preparations.
Flying after your operation
The other thing that comes up not infrequently is holidays and timing of holidays and flying.
If you can avoid travelling, air travel in particular, in the first six weeks is sensible.
If you do travel you may need to take extra agents to reduce blood clot risk such as aspirin but you should consult your GP about this.
Pre-operative assessment clinic
Before the operation you may be called to a Pre-Operative Assessment Clinic for an assessment.
More frequently nowadays this may happen on the same day as being seen. In other cases, it will happen nearer to the time of surgery.
This may be carried out by a specialist nurse or an anaesthetist and this is an opportunity to check your blood pressure, carry out a heart tracing, chest X-ray as necessary and perform blood tests and to do a blood grouping and typing. If you do need blood, then that has already been taken care of.
This is to reduce any potential for late cancellation to make sure that all your physiological parameters are considered. You may or may not see the anaesthetist.
If there are particular risks, then you may require further investigation such as for example an echocardiogram if there is concern about your heart and there may be a necessity to take further blood readings if you are hypertensive. The anaesthetic nurse may consult with the anaesthetist.
Type of anaesthetic
Patients quite often ask about the anaesthetic, will they have a general anaesthetic, a spinal, or an epidural?
A general anaesthetic is when you have an injection and basically you go to sleep. With a spinal anaesthetic or an epidural, a needle is placed into the back and your legs are made numb.
The spinal tends to be a one-off injection of anaesthetic which is good for shorter procedures whilst in an epidural a tube(catheter) is left in and drugs can continue to be administered after surgery for prolonged pain relief. These types of anaesthetic are very effective for several reasons. They do control blood pressure very effectively which often reduces intraoperative bleeding. It is quite good at providing good haemodynamics, which potentially reduces blood clot risk and probably even more importantly, it does provide very good post-operative pain relief.
However, there are different trends and recommendations and some surgeons are using infiltrations of local anaesthetics combined with a general anaesthetic, so practice does vary and it is important to discuss this with your surgeon or anaesthetist to understand what you are having.
Sometimes, pain relief is administered by a pain-pump locally into the wound postoperatively or by pushing a button to administer safe doses of painkillers - called patient controlled analgesia (PCA).
Some patients have a fear of not waking up and therefore wish to be awake and it is possible to have a spinal and stay very alert and even potentially talk to the anaesthetist and surgeon doing the operation but, equally, it is possible to be sedated with a spinal, so don’t think you must stay awake if you have a spinal anaesthetic.
What happens in hospital?
When will I be admitted?
Patients traditionally came into hospital the night before the operation but there is an increasing trend to come in on the day of surgery. This of course, does depend to some extent on the age and faculty of the patient and to some extent where they live but if you do come on the day of surgery all the tests will have been done beforehand.
How long will I be in hospital?
The length of stay following surgery is variable. It may be in some circumstances as short as three days and quite often five days, may be seven days on occasions. There are instances of patients being discharged on the same day as but this is not the accepted routine. Do not feel rushed and the most important factor is to make sure the whole process is acceptable for you and there is a gradual and safe transition, either back to intermediary care or to your home circumstances.
Nil by mouth
If you come in on the day of surgery you will need to come in possibly starved, i.e. not having anything to eat or drink from midnight but you will be told of the exact timing. You may need to come to the hospital early.
Immediately prior to surgery
When you come into the hospital you will be checked by the hospital and ward staff and shown to your room. You may take a shower prior to the operation and be placed in a surgical gown. You should be seen by the surgeon operating on you, or a representative of the surgeon, for the consent form to be signed and your leg marked. The leg is normally marked very close to the hip or knee so that it can be seen when you go to the operation for surgery.
Getting to theatre
Some hospitals you walk to the operating theatre or are pushed in a chair. Less frequently now patients go down on a bed or a trolley. When you leave the ward all your details are cross checked by the nurse handing over to the porter, if a porter is used, and once you go into theatre a second check occurs, checking your name, your armband, any allergies and what operation you are having.
In the anaesthetic room
When you go into the operating room you will be shown into the anaesthetic room where you will be seen by the anaesthetist. In fact, the anaesthetist will probably have seen you earlier on either before or after the surgeon has seen you.
You will have had a Venflon tube and/or drip inserted into your arm so fluids can be replaced during the operation. With regard to your position, if a spinal anaesthetic is to be used you will be asked to sit on the table bending slightly forward so that the injection can be given. Once the anaesthetic takes effect you will be positioned either on your back or the side depending on the surgical technique and you may be draped up and prepped in the anaesthetic room prior to coming into theatre but practices do vary.
In theatre
Once you are taken into theatre a re-draping is often carried out whereby the leg is isolated from the rest of the body with sterile drapes and quite often a curtain is put up from just above the waist up to exclude the top end of your body and the anaesthetic and other personnel from the wound. Very commonly we use special theatres with ultra-clean air and very high ventilation and air flows and there is quite often a slight noise or hum from the Air Flow system and the air can be slightly cool. The temperature in theatre is controlled to about 20 degrees so it is reasonably comfortable but if you are cold then various devices can be used to ensure that your body temperature is maintained. Surgery is then carried out which normally takes about 60 to 80 minutes although it does vary depending on exactly what you are having done.
In recovery
You will have an oxygen mask or nasal cannula to ensure adequate oxygenation and then following the operation, you may be in the Recovery area for a short period of time where you will be monitored by one of the anaesthetic staff to make sure all your physiological parameters, i.e. your pulse and blood pressure are acceptable and pain relief is controlled before going back to your room or your ward. There will be a dressing on your leg. You may well have a urinary catheter in place if a spinal anaesthetic has been used because after the spinal bladder function can be abnormal for a period of time. You may or may not have a drain in place. Surgeons have different philosophies about using drains which is a tube coming from the wound to drain blood out although there is an increasing trend not to use a drain. You may well have a check X-ray in the recovery although more commonly these X-rays are taken later on.
Back on the ward
To reduce the risk of blood clots you may have a daily injection of low molecular weight Heparin and you may well also have a mechanical device applied to either your foot or your calf to cause a pumping action to pump blood from the leg back to the heart keeping the blood circulation going to reduce the blood clot risk. You will also be asked to do calf muscle exercises to help pump blood back up the limb. You will also receive intravenous antibiotics after surgery to help prevent infection.
Getting going after surgery
There are some practices of very early mobilisation. In fact, there are stories of some patients even walking back from the Recovery Room, particularly in patients staying in hospital just a day or two. This seems to be more popular in the US where there is a strong drive to reduce inpatient stay. However, we would stress that this is not the norm, particularly in the UK and most patients don’t mobilise until the day following surgery.
You will be monitored overnight and the next day you will be seen and checked over by the nursing staff and by the physios. Normally patients will be standing within 24 hours and then will progress to walking, either with a Zimmer frame or with crutches over the next day or so. Initially, this will be with assistance and then eventually by yourself. You will progress through various stages - being able to transfer from bed to chair, going to the toilet and back and going to the shower and gradually becoming independent, walking down the corridor and being able to go up and downstairs with instruction. This process takes three to five days depending on many factors such as type of surgery, age and preoperative fitness.
You will have various checks to make sure all is well and there are various protocols to be adhered to. When it is safe for you to go home you will normally be allowed to go home in a car.
Do I need any aids or appliances?
We have normally in the past assessed patients for any additional aids by the Occupational Therapist and these sometimes include a raised toilet seat and assistance to get shoes and socks on and possibly even alterations to furniture at home. The principle is to ensure that the furniture is not so low that the hip is abnormally flexed which could introduce a dislocation risk.
There is some variation in terms of how many appliances are needed but at the moment it is still fairly common to have some appliances provided for about six weeks after the operation and in some cases these appliances can be supplied and indeed fitted if necessary prior to the operation, although most of these appliances are easily fitted and are quite simple and modular.
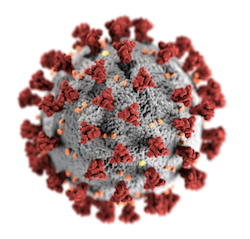
COVID-19
The impact of COVID-19
As the patient, you are the most important member of your healthcare team and it is always a good thing to feel informed and empowered to take an active role in your care.
The added risks posed by the coronavirus pandemic mean that there is now more to be aware of and that you have a greater role to play. You may have a different experience from what you might have expected, with additional challenges both before and after surgery.
The weeks before surgery is a time to prepare mind, body and home for the operation and the postoperative recovery.

Under the current circumstances, significant precautions need to be taken by both you and us to reduce the risks of COVID-19. By reading this and informing yourself about the situation and what you can do, you are already taking a positive step.
The other key steps that you will need to take before surgery are to:
- Have a COVID-19 test swab before surgery, as advised by your healthcare team
- Follow the self-isolation and/or ‘shielding’ plan from your team
- Inform your team if you, or anyone you are isolating with, develop symptoms of COVID-19
- Avoid public transport, wear a mask and observe social distancing when travelling to hospital
The purpose of these precautions is to protect you and to reduce the risk of introducing the virus into the hospital.
We will endeavour to keep the information here on this website and in the myrecovery app up-to-date with the latest guidance. However, the recommendations around COVID-19 may change and, as with all the resources here in the app, please do not rely on these articles over any advice given to you by a healthcare professional or a member of your healthcare team.
More information is available on The British Orthopaedic Association website.
If you have any serious concerns at any point, please contact my office and my team and I will be happy to assist you.
Video: The risks of COVID-19
This video is a segment from a longer session on the possible complications and risks for hip replacement recorded for Joint School Live.
Extra measures before and after surgery
The extra measures that need to be taken may include:
Testing before surgery
To help ensure that the virus is not brought into the hospital, you will be required to be tested for COVID-19 before your operation.
You will be given instructions as to how, when and where the test swab can be taken, such as via a ‘drive-thru’ facility.
Please be aware that not following the COVID-19 testing instructions from your healthcare team could result in your operation being postponed.

Self-isolation or shielding
Depending on the details of the procedure and personal risk factors, some people will be advised to self-isolate with their household or shield within their household for a certain number of days before surgery.
Social distancing before surgery
Some hospitals will be separated into different zones, if this is the case, you will be given clear directions as to where you should arrive on the day. Please avoid using public transport to travel to or from the hospital. If you do not have a means of transport, please contact your team so that this can be arranged. Wear a face mask while travelling and wash your hands thoroughly before and after.
If you, or anyone you live with, experience any symptoms of COVID-19 in the days before surgery, please inform your team.
The symptoms of COVID-19
COVID-19 affects different people in different ways.
If you think you or anyone you are self-isolating with have developed a symptom of COVID-19, please contact your healthcare team.
More common symptoms of COVID-19 include:
- Fever
- Dry cough
- Tiredness
Less common symptoms include:
- Aches and pains
- Sore throat
- Diarrhoea
- Conjunctivitis (red or pink eyes)
- Headache
- Loss of taste or smell
- A rash or discolouration of fingers or toes
If you experience any serious symptoms, such as difficulty breathing or chest pain, seek immediate medical attention.
In most cases, people experience a mild to moderate illness and recover without needing any medical care or hospital treatment.
People with mild symptoms who are otherwise healthy should manage their symptoms at home.
Self-isolation or shielding before surgery
To reduce exposure to the virus that may be circulating in the community, some people will be advised to stay at home for a certain number of days before the procedure.
Initially, 14 days was selected as the duration, based on evidence that 99% of patients will develop symptoms of COVID within 14 days of being infected.
This guidance has since been updated and the advised duration of self-isolation may be reduced, but this will depend on individual risk factors.
Self-isolating with your entire household
In some cases it will be preferable to self-isolate with your whole household, meaning that no one that you live with can leave the house but you can interact with one another as normal. If you have the benefit of a private garden, this can be used by members of the household.
All members of the household must observe social distancing when receiving deliveries or answering the front door.
Please report to your healthcare team if you or anyone in your household develops symptoms of COVID.
If you have been advised to self-isolate and are unable to work during this period, you may be entitled to sick pay.
Shielding within your household
With shielding, the rest of the household are relatively unaffected but the person awaiting surgery distances themselves from others in the home to reduce exposure to the virus.
This means keeping 2 metres (3 steps) away from the people you live with and practicing good hand hygiene. Minimise the time other people living with you spend in shared spaces such as kitchens, bathrooms and sitting areas, and keep shared spaces well ventilated.
Use separate towels from the other people in your house and, if possible, use a separate bathroom. If you share a toilet and bathroom with others, it’s important that they are cleaned every time after use (for example, wiping surfaces you have come into contact with). Consider drawing up a rota for bathing, with you using the facilities first.
If you share a kitchen with others, avoid using it while they’re present. If you can, take your meals back to your room to eat. If you have one, use a dishwasher to clean and dry the family’s used crockery and cutlery. If this is not possible, wash them using your usual washing-up liquid and warm water and dry them thoroughly. If you are using your own utensils, remember to use a separate tea towel for drying these.
Everyone in your household should regularly wash their hands, avoid touching their face and clean frequently touched surfaces.
If any member of the household experiences symptoms of COVID during the shielding period, please inform your healthcare team to discuss and evaluate the risk of infection even with distancing precautions in place.
Shared decision-making and informed consent
Having an operation is a shared decision made together with your surgeon.
To make an informed decision, you need to be satisfied with your understanding of the intended benefits; the possible risks; alternative treatments and the consequences of not having the procedure.
The impact of COVID-19 means that your care pathway will be different from what it would have been. For example, access to face-to-face postoperative appointments and/or rehabilitation is likely to be reduced.
At the time of writing, the added risks posed by COVID-19 are difficult to quantify. The additional risks of having a COVID-19 infection during the postoperative phase will be discussed.
The information, checklists and surveys in the myrecovery app will aim to assist this process and serve to complement the conversations with your surgeon and other members of your healthcare team.
The statements below have been put together to help to support your informed consent, please consider each one before your procedure and ask your team if you have any questions.
-
I am satisfied with my understanding of what the planned procedure involves
-
I am aware of the intended outcome; the likelihood of success and of potential follow-up treatments
-
I am aware of the risks associated with the procedure and what these may mean for me, in terms of my work, hobbies and quality of life
-
I am aware of alternative treatments, including non-surgical options
-
I understand how my condition might develop without treatment and how lifestyle choices could affect the progression of my symptoms
-
I understand that I will have the opportunity to discuss the details of anaesthesia with an anaesthetist before the procedure
-
If having surgery in an NHS hospital, I understand that another surgeon other than my Consultant may perform the operation (although they will have adequate training and/or supervision)
-
I understand that any procedure in addition to what my surgeon has described on the consent form will only be carried out if necessary to prevent serious harm to my health