Hip surgery
There are many types of surgery that can be performed on the hip. Some of the more common operations are detailed here.
Total Hip Replacement (THR)
Total hip replacement was developed and pioneered by Professor Sir John Charnley, an English surgeon working in the north west of England in the 1950s and 1960s. Prior to Charnley’s contributions the methods used to address hip arthritis were fairly rudimentary and the functional results and pain relief were not particularly good.
Charnley carried out this work at Wrightington Hospital which is now the Centre for Hip Surgery near Wigan in Lancashire. The hospital is still active in carrying out all forms of joint replacement surgery and that has now extended to other joints such as the ankle and upper limb joints including the shoulder, elbow, wrist and hand joints.
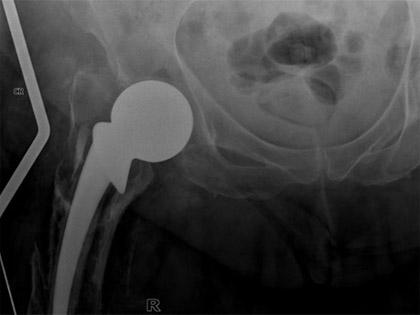
The principles of total joint replacement remain very similar to those advocated by Charnley. The operation consists of exposing the hip joint, removing the femoral head or ball joint, removing any remaining articular cartilage from the socket or acetabulum and inserting a new socket with or without cement into the acetabulum. A femoral component is inserted down the shaft or internal surface of the femur. Again, fixation is made by using acrylic bone cement (as advocated by Charnley) or by using a special coating which assists biological ingrowth into the femoral shaft.
The moving(articulating) parts of the hip replacement, the ball and socket, can be made in a variety of different materials with different wear characteristics. Originally and in fact still most commonly used is a metal femoral head made out of stainless steel or cobalt chrome articulating with a socket made out of surgical grade high density polyethylene. Other common combinations are a ceramic head on a polyethylene socket, a ceramic head on a ceramic socket and a metal head on a metal socket.
Image showing a Charnley hip stem, demonstrating the slightly rough surface of the stem and the 22.225mm metal head.

Image showing a polished, triple tapered hip stem, the C-stem. The design contrasts with the original Charnley by having a smooth, polished surface and is modular in that different head sizes can be used.

Image showing an uncemented hip stem (the Corail stem). The textured surface of this titanium stem is covered with a layer of hydroxyapatite to encourage the patient’s bone to grow onto the implant.

Image showing a different type of uncemented stem, the Zweymuller stem. A ceramic head is shown.

Image showing a ceramic on ceramic hip system (a Corail stem with a Pinnacle socket).

Image showing a ceramic on poly hip system (Charnley Elite Plus stem with cemented poly socket).

Image showing an uncemented socket with a poly liner.

Hip Stems Library
A library of images of femoral stems used in total hip arthroplasty.
Charnley

Charnley Extra Heavy

C Stem

Charnley Elite Plus

Corail (collared)

Corail (non-collared)

REEF (revision stem)

Zweymuller

Freeman

What can I expect after hip replacement surgery?
The main objectives of total hip replacement are:
- To substantially reduce pain (if not eliminate all pain)
- To maintain or improve range of movement
- To improve function, whether it be mobility or tasks such as walking, housework, shopping, exercise etc.
It is reasonable to expect virtually normal function for your age if all goes well, in other words ability to walk several miles unaided, to go swimming, to probably play golf if you are a golf player for example or recreational tennis.
You may experience occasional aching around the hip, particularly over the outer side - the trochanter. You should have a good range of movement but you may have slight limitations in terms of flexion and rotation. Most activities should be possible.
You must remember to be careful bending at the extreme to avoid dislocation. Dislocation is mainly a potential problem in the first 12 weeks but there is a low and persistent risk of dislocation several years later.
One must avoid very strenuous flexion and rotation of the hip. Remember that the end result is somewhat variable and depends on pre-operative health and function. There is a very good chance that you will be pleased with the improvement following surgery.
High activity levels such as extensive swimming, use of exercise bikes and use of the gym, particularly the cross trainer and various other devices should be possible in most patients who are otherwise fit and active, although it may be sensible to avoid very high activity levels such as road running.
Some patients, particularly younger patients, want to resume very active sports such as running, mountaineering and very occasionally contact sports. Skiing is another activity patients sometimes ask about. There are different perspectives regarding advice as to whether patients should engage in these activities.
In some patients who are otherwise fit and active it is possible to return to this activity but I think most people would accept that they do put the joint in some jeopardy both in terms of how long it lasts and how quickly it wears and therefore if an individual patient understands that and accepts that these activities may reduce the lifespan it is perhaps an individual decision the patient needs to consider but views amongst surgeons and patients will vary quite considerably regarding these more extreme activities.
Video - Too young for a new hip?
Am I too young for a new hip? And other frequently asked questions
In this Joint School Live video, we discussed how hip replacement surgery is becoming increasingly common in younger ages, as well as a wide range of other topics and questions, such as:
- When is the right time to have a hip replacement?
- How long can one expect to need to take painkillers after surgery?
- Activity after hip replacement surgery
Hip revision
A joint replacement is a mechanical device and like any mechanical device there is always a potential of mechanical failure. There are many different ways a hip joint can fail and require revision operation. Causes of failure often requiring a revision or re-operation include:
- Deep Infection
- Dislocation
- Fracture
- Wear
- Loosening
More rare causes include ceramic fracture and hypersensitivity reaction to the materials in the implant.
Dislocation
Dislocation is a process where the ball joint comes out of the socket. It is more likely to occur in the first 12 weeks following surgery before the deep tissues are fully healed. The incidence of dislocation does vary but in most large series it is in the region of 4 per cent although dislocation rates approaching 1 per cent or less are possible. Dislocation tends to occur suddenly either after bending or stretching too far or after a fall.
Common mechanisms that can cause dislocation are attempts to bend down and put shoes and socks on and possibly getting up from low seating. The mechanism therefore is normally of hip flexion and in most dislocations but not all the femoral head comes out at the back. It is common practice to simply reduce the dislocation under general anaesthetic but occasionally the hip can continue to dislocate and if it dislocates on more than three occasions then further operation to stabilise the hip is often considered but this decision does vary from patient to patient depending on other features.
Another method of treating the dislocation either at the first or second occasion is to apply a hip brace to try and stabilise the hip.
X-ray showing a dislocated hip replacement

X-ray showing the same hip but now reduced with a posterior lip augmentation device (PLAD) attached to the socket to prevent further dislocation.

Fracture
Occasionally a fracture may occur around the prosthesis because of a severe trauma such as a road traffic accident or a fall.
The fracture may compromise the fixation of the hip replacement or else the fracture may be below the fixation of the implant.
The ways of treating it, if the hip is loose to treat the fracture and the loose hip all at one go. If the hip is not loose, it is sometimes possible just to plate the fracture.
X-ray showing a fracture around a hemiarthroplasty.

X-ray showing the fracture treated with removal of the implant and insertion of a longer uncemented implant with stabilisation of the fracture around the stem with cerclage wires.

Hip wear
Wear occurs because of the movement of the femoral head against the polyethylene and very small shards of material are released every step. These particles often are very small in the region of a micron or less and the material is taken up by cells called macrophages and over time when enough material is accumulated the cells are essentially overloaded with release of various chemicals (cytokines) which cause secondary effects on the bone and can be associated with loosening.
Loosening
The implant is fixed to the bone either with bone cement or by biological fixation but the stresses at the implant-bone interface are substantial and bone remodels with time.
Also, wear from the articulation, particularly the metal-plastic articulation, small particles of polyethylene can cause bone resorption with subsequent loosening of the socket and/or the stem (link to example cases of revision for loosening).
Hip resurfacing
Sir John Charnley, when pioneering hip replacement in the late 1950s and early 1960s, did initially try a resurfacing procedure.
He used materials (Teflon) to recap or resurface the ball joint and also to re-line the socket.
However, these failed fairly early on in a matter of a year or two because the material shredded debris which caused bone resorption.
This led Sir John to consider different materials and more robust methods of fixation. For that reason, Charnley used acrylic bone cement to fix components more securely to bone (the reason for the stem or shaft of the component going down the internal part of the bone) and also used different materials of metal on plastic.
However, other surgeons subsequently reconsidered resurfacing using perhaps better materials in terms of material, design and fixation and various pioneers such as Freeman from the London Hospital, Amstutz from Los Angeles and more recently McMinn from Birmingham have reconsidered and reintroduced resurfacing. The Birmingham hip resurfacing introduced by McMinn from 1996 onwards has led to a rekindled interest in hip resurfacing. McMinn started experimenting with different methods of fixation from 1991 but by 1996 had settled on an uncemented porocoat acetabular component articulating with a metal femoral component cemented onto the femoral head.
A Birmingham hip resurfacing implant

This bearing is a metal on metal cobalt chrome articulation which has extremely low wear properties compared to the conventional metal on plastic although the wear debris material is a lot smaller.
The potential advantages of a hip resurfacing are stated as follows:
- Less invasive - involves taking less bone off the femur.
- Should it be necessary to revise a resurfacing more bone is available and therefore potentially easier to revise.
- Quicker recovery.
- Better activity.
However, there are also potential disadvantages.
- May take slightly more bone off the acetabular side of the hip joint (this is a factor disputed in some scientific papers).
- A risk that the femoral neck may fracture (a fact substantiated in the literature - incidence of 0.5 to 1.5%).
- Effects of the release of material from the metal bearing - mainly cobalt and chromium metal ions.
- Function may not be good as a standard hip replacement because of the potential of the femoral neck abutting or impinging on the rim of the acetabulum, particularly in flexion.
As yet, we have limited information on the medium to long term outcomes of resurfacing versus total hip replacement. The short-term results from large epidemiological studies - joint registries particularly from Australia - would indicate a higher failure rate within the first three years of resurfacing compared to patients undergoing hip replacement. It remains to be seen what the comparable outcomes will be at 10 years and 20 years which are the longer benchmark figures for joint replacement surgery.
Other unknowns about hip resurfacing - the incidence of late collapse of the femoral head, the fate of neck thinning (see X-ray) and potential local reaction to metal - ALVAL (aseptic lymphocytic vascular and associated lesions). ALVAL is not yet fully understood but tends to present as pain and occasional swelling around the hip. X-rays are often normal but the swelling can sometimes be seen using a special form of MRI scanning (MARS- Metal Artefact Reduction Scan).
The proportion of patients developing this problem is, as yet unknown but latest reports (March 2010) suggests an incidence of between 1% and 6% depending on age and gender. The extent of the metal reaction can vary from a minor reaction to fluid collections to more extensive tissue swellings (pseudotumors).
We have had some experience at dealing with this problem and it appears that revision of the components to a non-metal-on-metal articulation appears to treat the pain satisfactorily, particularly if treated early. Research in this field is continuing.
It is not clear at present whether this condition is a hypersensitivity type reaction (type of allergy) or a normal reaction to an abnormal load of metal ions, although it is likely that high wear/ high local metal ion levels are the predominant contributing factor.
X-ray showing neck thinning in a patient with a hip resurfacing

There are some concerns regarding the longer-term effects of very small cobalt and chromium accumulation in the rest of the body. The cobalt and chromium is dissipated in the bloodstream in the lymphatics and very small traces can be found in distal organs, namely the spleen, liver and even the brain and although the concentrations are quite small we do not yet fully know the long-term consequences of it.
There are some studies that suggest there may be some chromosomal changes in patients who are exposed to metal ions. The question of late oncological or cancer risks have been looked at and as yet looking at cancer registries, particularly from Scandinavian countries, there is no evidence that there is an increased cancer risk in patients exposed to metal on metal articulations but authorities debate whether the scientific data is completely robust at this stage.
Other potential risks include that of teratogenesis, i.e. birth defects in children. It is known that small amounts of metal can be transferred across the placenta from the mother to the child. As yet there are no known cases of teratogenic effects but again, this has been questioned by some authorities and as such some surgeons do not recommend resurfacing in females who may wish to consider having a family.
Hip arthroscopy
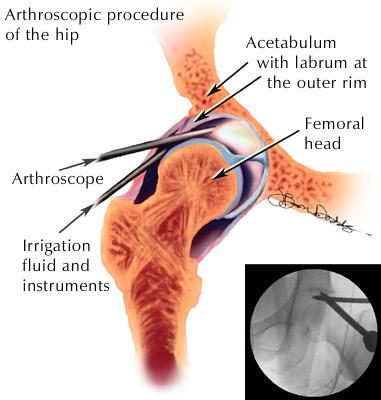
What is hip arthroscopy?
Hip arthroscopy is key-hole surgery on the hip joint. It is performed through small (2cm) incisions using a camera to visualise the inside of a joint. Traction is needed to create a space in the hip to insert the instruments.
Patients with the following problems can benefit from hip arthroscopy:
Labral Tear
The labrum of the hip is a lip of thick cartilage that runs around the edge of the hip socket. When a labral tear of the hip occurs, the torn tissue can become pinched in the joint causing pain and catching sensations. Labral tears can occur from acute injuries such as sport or as a chronic problem due to impingement of the hip.

A labral tear of the hip seen from the arthroscope.
Hip impingement
Impingement of the hip is when the shape of the hip bones causes repetitive injury to the labrum and the cartilage lining the joint. This results in hip pain and may be one of the factors that lead to arthritis.
Treatment involved reshaping of the bones inside the hip. Sometimes cartilage within the hip is also affected and this can be treated at the same time (See the FAI page for more info). The following video shows how hip arthroscopy can treat the abnormal shape of the femoral head by reshaping, often called femoral osteochondroplasty.
Loose Bodies
Loose bodies are pieces of cartilage that form within the joint. They look like small marbles floating within the joint space. These loose bodies can become caught within the hip during movements.
Snapping Hip Syndrome
Snapping hip syndrome has several causes, some of which can be treated with hip arthroscopy. If something is catching within the hip joint, hip arthroscopy can be used to relieve this snapping. Also, hip arthroscopy can be used to perform a psoas tendon release in cases of internal snapping hip syndrome.
Diagnosis
Most of the hip conditions that can be treated with hip arthroscopy present with either groin pain, buttock or thigh pain and sometimes with mechanical symptoms of clicking, catching or snapping in the hip which can be painful. Duration of symptoms can vary from only a few weeks after an injury to many years.
Often patients have consulted many different doctors before referral is forthcoming. One of the diagnostic difficulties is that standard X-rays of the hip are generally normal and often MR arthrogram of the hip is used to investigate these problems.
The symptoms described above can often be precipitated during examination by so called impingement testing - that is flexion to 90 degrees and internal rotation of the hip. Other movements during examination of the hip can also precipitate pain or clicking.
What are the possible complications from hip arthroscopy?
Complications following hip arthroscopy are uncommon. However, the most concerning have to do with several important nerves and blood vessels that surround the joint. Nerve injury is uncommon, but can be a significant problem. The most commonly affected nerves include the lateral femoral cutaneous nerve (sensation to the thigh) and much less commonly the sciatic nerve. Injury to any of the nerves can cause pain and other problems.
Other possible complications from hip arthroscopy include infection, blood clots, traction injuries and continued pain after the surgery. one exceptionally rare but devastating complication is AVN of the femoral head (bone death due to interrupted blood supply) leading to hip replacement. The rate of these complications is low, but patients need to understand the potential risk prior to undergoing a hip arthroscopy.
Rehab after hip arthroscopy
In the first few weeks after surgery, patients are often instructed to keep some weight off the hip, particularly if the bone has been reshaped. Work on regaining motion around the joint, and gentle strengthening exercises start early on. Typically, patients work with a physiotherapist for advice with exercises and stretches.
Most patients can begin light activities (cycling, swimming) within a few weeks. Athletes most often take about 12 weeks to start more rigorous training. Full recovery can take 6 months and is dependent on the duration of symptoms before surgery.
Benefits for patients
Hip arthroscopy has been proven in published papers to be effective at relieving pain from labral tears, loose bodies and impingement. The patients that do not do so well are those with significant arthritic change and hip replacement may be more appropriate depending on the level of symptoms.
References: Philippon et al JBJS 2009;91B:16-23